EMDR and the adaptive information processing model . KH 2020
The theory behind emdr is based on how information is processed in the brain. With happy or everyday events information is processed in an adaptive way
The brain works like a library. Imagine that an event is like a piece of paper to be filed. It contains details of our thoughts or feelings, the description of the events using all our senses together with our cognitions about the event.
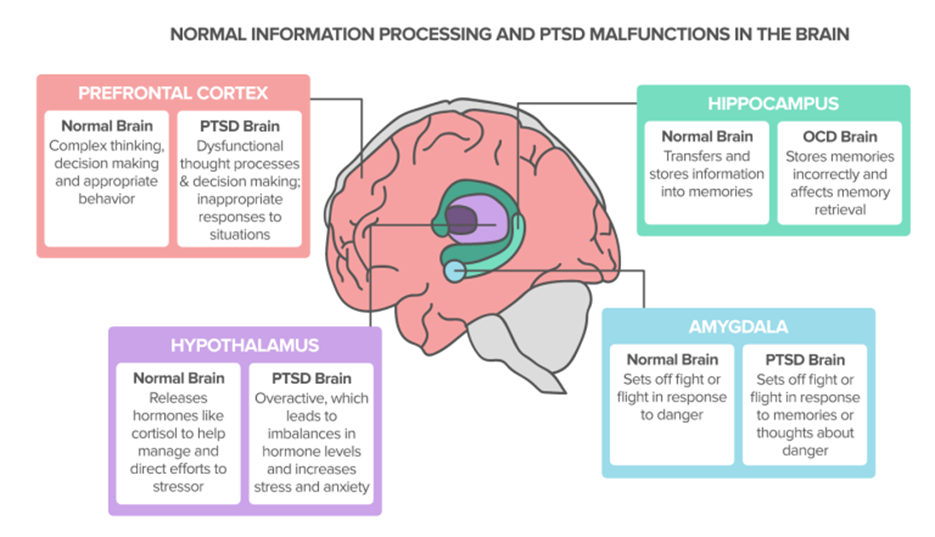
This is received by the limbic system our emotional brain centre. The limbic system contains the amygdala which is like the smoke detector and detects level of emotional disturbance and the hippocampus which access the librarian. When an event is not too disturbing, the librarian is able to identify relevant hashtags so it can find the relevant brain networks/ files and sub files in the library to the event can not only be filed as a memory but a piece of learning experience. Eg ice cream on a sunny day with mum, #mum, #icecream, #sunshine
In an everyday event the disturbance isn’t assessed by the amygdala as being too emotional or disturbing so the event is able to be chronologically filed by the as a memory this is how information is processed adaptively.
However when there is traumatic or distressing event, there is a huge emotional content and so the piece of paper to be filed will be full of fragmented information. There will be huge emotional content and all the senses will be heightened so it cant be written into a coherent storey. This overwhelms the amygdala and so events are not passed as adaptive but maladaptive and therefore not filed.
Another important factor is the amygdala and hippocampus a timeless, there is no time frame so if information doesn’t get passed to be filed because it’s maladaptive then it will the elements will recur in real time. So you might get flashbacks of the sights or the sounds or triggered by certain elements that have not been filed away.
So emdr works by kick starting the bilateral ability of the brains natural ability to adaptively process information by taxing the working memory so it no longer can hold emotionally intense data. It enables the original information on your A4 paper to be organised in a way that the brain can process it by working through the fragments and making sense of them, so the client moves from an emotional aroused state to adaptive appropriate emotional grounded state.
The Effects and Treatment for Prolonged Stress and Trauma Kim Harries July 2019
Traumatic Stress Relief Instruction Videos – Traumatic Stress Relief (TSR) (1stcontact.net)
Prince Harry is doing a special trauma therapy called EMDR. It worked for me
https://www.theguardian.com/commentisfree/2021/jun/16/prince-harry-is-doing-a-special-trauma-therapy-called-emdr-it-worked-for-me?CMP=Share_iOSApp_Other
Dis-stress affects us neurologically, physically, emotionally and psychologically,
Neurology-What is the science of psychological shock?
The fight, flight or freeze response is actually physiological and biochemical. Meaning a lot goes on for our bodies and it’s far from ‘in your head’.
Difficult and overwhelming experiences trigger the limbic system in the mammalian brain and cause the older brain, often called the ‘lizard brain’ or ‘reptilian brain’, to take over. We experience what is called ‘flight, fight, or freeze mode‘, or, more scientifically, an ‘acute stress response’.
Fighting, fleeing, or freezing (so a predator passed us over) surely served us well when we were cave people faced with wild animals. And an acute stress response gives us the energy required to make fast decisions in the face of life-threatening things such as natural disaster, crime, and physical attacks.
Physical – What is going on in your body and brain to cause all this?
In the aftermath, moods can swing wildly, you can feel anxious and socially withdraw, and you might not be able to cope with day-to-day life. Physical symptoms include fatigue, muscle tension and feeling flu-like. You may also:
Have trouble functioning at home or work
Suffer from severe fear, anxiety, or depression
Be unable to form close, satisfying relationships
Experience terrifying memories, nightmares, or flashbacks
Avoid anything that reminds you of the trauma
Feel emotionally numb and disconnected from others
Use alcohol or drugs to feel better
Psychologically – What does stress do to your mind?
Your sense of self and core beliefs will be knocked. As a result of the stress or trauma, you may feel responsible, a failure, powerless and impotent. It could shake your faith in others and make you question your beliefs, morals and integrity. Talking this through with a specialist and loved ones enables you to acknowledge and recognise these feelings and gradually rebuild you world view.
Intrusive thoughts and memories. After a traumatic event, it is common to experience some intrusive thoughts and memories of the traumatic event. This is especially likely to occur when you encounter something (for example, a person, place or image) that reminds you of the traumatic event.
Hypervigilance. It is also very natural to feel more on-guard and aware of your surroundings after a traumatic event. This is actually a very protective symptom following a traumatic event. Your body is attempting to keep you safe by making you more aware of potential sources of threat and danger. This natural safety mechanism is going to be more sensitive after a traumatic event is experienced.
Hyperarousal. Just as you are going to likely be more on-guard, you are also likely going to feel more keyed-up and on edge following a traumatic event. This is again part of your body’s natural protection system. Fear and anxiety tell us that there is some kind of danger present, and all the bodily sensations that go along with fear and anxiety are essentially designed to help us respond to that danger. They are preparing us to flee, freeze or to fight. Following a traumatic event, your body’s alarm system is going to be more sensitive in an attempt to protect you from future traumatic events.
Feeling Unsafe. After a traumatic event, our assumptions about the world being a safe and secure place are understandably shattered. Consequently, people may feel as though any situation or place is potentially dangerous. Places or situations you once felt secure in may now feel threatening and be anxiety-provoking. This is especially likely to occur in situations or places that remind you of your traumatic event.
Dissociation, disconnection. You may also find yourself zoning out. This is a defence mechanism than enables you to cope with all the sensory input that your brain is having to deal with as you heal.
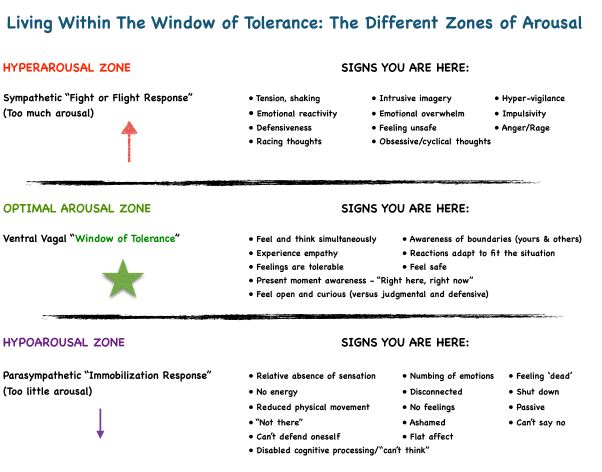
RATE YOUR STRESS FROM
0 -+10, +10 is hyper arousal (Anxiety),
0 – -10, -10 is hypo arousal (depression).
Anything out of the 5s means we are out of your Window of Tolerance and you need to TAKE ACTION….
Other Psychological and physical reactions include:
Loss of interest. It is important to keep an eye out for a loss of interest in activities that you used to once enjoy, as well as feelings of being detached from others. This symptom can be a sign that you are at risk of becoming depressed. This symptom may also cause you to isolate yourself from others, including important sources of social support.
Avoidance. After a traumatic event, it is very common to avoid certain situations, activities or people. However, you must pay attention to avoidance behaviours. Avoidance usually leads to more avoidance as it reinforces our beliefs that the world is not a safe place after a traumatic event. This avoidance can then lead to a worsening of symptoms and eventually PTSD.
Unhealthy coping behaviours. Just as avoidance of activities, situations or people can be problematic, so can the avoidance of thoughts and feelings. The symptoms people experience after a traumatic event can be very distressing. As a result, people may rely on unhealthy coping strategies (for example, using substances) as a way of avoiding these symptoms. Avoidance is only a short-term solution, and in the long-run, it can actually cause your feelings and thoughts to become more intense. You may experience
PTSD, Anxiety and Depression. Symptoms of Post Traumatic Stress Disorder & C-PTSD
The symptoms of PTSD and C-PTSD can have a significant impact on your daily life.
Each person’s experience of PTSD is unique to them and people react to traumatic experiences in a variety of ways: you might have experienced a similar type of trauma to someone else, yet be affected in a different way.
Many people who experience a trauma will experience some symptoms which dissipate after a number of weeks. However if those symptoms continue for longer than a month, and are affecting your day-to-day life, PTSD or C-PTSD may be present. In around 15% of people, there may be a delay of months or even years before symptoms even start to appear.
PTSD and C-PTSD symptoms can vary in intensity over time. Some people with PTSD learn to ‘manage’ their symptoms and so have long periods when their symptoms are less noticeable, followed by periods where they get worse. Other people have constant severe symptoms, or you may only have symptoms when you’re stressed in general, or when you run into reminders of what you went through.
PTSD and C-PTSD symptoms vary from person to person, but these are some common signs and symptoms that you might recognise:
Re-experiencing Symptoms
Re-experiencing is the most typical symptom of PTSD & C-PTSD. This is when a person involuntarily and vividly relives the traumatic event
Flashbacks—reliving the traumatic event, and feeling like it happening right now including physical symptoms such as a racing heart or sweating
Reoccurring memories or nightmares related to the event
Distressing and intrusive thoughts or images
Physical sensations like sweating, trembling, pain or feeling sick.
Thoughts and feelings can trigger these symptoms, as well as words, objects, or situations that are reminders of the event.
Avoidance Symptoms
Trying to avoid being reminded of the traumatic event is another key symptom of PTSD & C-PTSD: avoiding certain people or places that remind you of the trauma, or avoiding talking to anyone about your experience.
Staying away from places, events, or objects that are reminders of the experience
Feeling that you need to keep yourself busy all the time
Using alcohol or drugs to avoid memories
Feeling emotionally numb or cut off from your feelings
Feeling numb or detached from your body
Being unable to remember details of the trauma
Avoidance symptoms may cause people to change their routines.
Alertness and Reactivity Symptoms
You may be ‘jittery’, or always alert and on the lookout for danger. You might suddenly become angry or irritable.
Being jumpy and easily startled
Feeling tense, on guard, or “on edge” – this is called hypervigilance
Having difficulty concentrating on even simple and everyday tasks
Having difficulty falling asleep or staying asleep
Feeling irritable and having angry or aggressive outbursts
Self-destructive or reckless behaviour
Aversion or difficulty in tolerating sound
Feeling and Mood Symptoms
The way you think about yourself and others may change because of the trauma.
Trouble remembering key features of the traumatic event
Feeling like you can’t trust anyone
Distorted thoughts about the trauma that cause feelings of blame and guilt
Overwhelming negative emotions, such as fear, sadness, anger, guilt, or shame
Loss of interest in previous activities
Feeling like nowhere is safe
Difficulty feeling positive emotions, such as happiness or satisfaction
A diagnosis of C-PTSD includes the same symptoms of PTSD, but also has 3 additional categories of symptoms: difficulties with emotional regulation, an impaired sense of self-worth, and interpersonal problems such as:
constant issues with keeping a relationship,
finding it difficult to feel connected to other people,
constant belief that you are worthless with deep feelings of shame and guilt
constant and severe emotional dysregulation (you find it difficult to control your emotions).
Why do PTSD & C-PTSD have physical symptoms too?
‘When we feel stressed emotionally, our bodies release hormones called cortisol and adrenaline. This is the body’s automatic way of preparing to respond to a threat, sometimes called the ‘fight, flight or freeze‘ response.
Studies have shown that someone with PTSD will continue producing these hormones when they’re no longer in danger, which is thought to explain some symptoms such as extreme alertness and being easily startled.
Some people also experience physical symptoms similar to symptoms of depression and anxiety, such as headaches, dizziness, chest pains and stomach aches, low mood, suicidal ideation.’
These altered cortisol levels also cause other physical symptoms such as your skin scaring more easily, digestive issues, and cold hands & feet, find out more in our blog article, ’10 unexpected physical symptoms of PTSD’ here.
Healing from Stress
Stress and trauma symptoms typically last from a few days to a few months, gradually fading as you process the unsettling event. But even when you’re feeling better, you may be troubled from time to time by painful memories or emotions—especially in response to triggers such as an anniversary of the event or something that reminds you of the trauma.
Tip 1: Validate your feelings.
You don’t have to force yourself to talk to others about how you feel; however, it is important you don’t try to push away your feelings. Allow yourself to feel what you feel when you feel it. Acknowledge your feelings about the trauma as they arise, talk abou them and accept them.
Tip 2: Take care of your health
It’s true: having a healthy body can increase your ability to cope with the stress of trauma.
Exercise. It turns off the limbic system
Get plenty of sleep. After a traumatic experience, worry or fear may disturb your sleep patterns. But a lack of quality sleep can exacerbate your trauma symptoms and make it harder to maintain your emotional balance. Go to sleep and get up at the same time each day and aim for 7 to 9 hours of sleep each night.
Avoid alcohol and drugs. Their use can worsen your trauma symptoms and increase feelings of depression, anxiety, and isolation.
Eat a well-balanced diet. Eating small, well-balanced meals throughout the day will help you keep your energy up and minimize mood swings. Avoid sugary and fried foods and eat plenty of omega-3 fats—such as salmon, walnuts, soybeans, and flaxseeds—to give your mood a boost.
Reduce stress. Try relaxation techniques such as meditation, yoga, or deep breathing exercises. Schedule time for activities that bring you joy such as your favourite hobbies.
Tip 3: Self-regulate. Switch off your nervous system
No matter how agitated, anxious, or out of control you feel, it’s important to know that you can change your arousal system and calm yourself. Not only will it help relieve the anxiety associated with trauma, but it will also engender a greater sense of control.
EMDR Anchor. Butterfly hug, hug and tap left right left right, Tap feet, left right left right. Practise o you’re anchor with left right tapping.
Mindful breathing. If you are feeling disoriented, confused, or upset, practicing mindful breathing is a quick way to calm yourself. Simply take 60 breaths, focusing your attention on each ‘out’ breath. Breathe in and out slowly through your nose practise so that each breath last up to 7 seconds. Box breathing in for 4, hold for 4r, out for 4, rest for 4. Practise diagram breathing.
Distraction. Notice your surroundings. Count five thigs, then 4, then 3, then 2, then 12. Does a specific sight, smell or taste quickly make you feel calm? Or maybe petting an animal or listening to music works to quickly soothe you? Everyone responds to sensory input a little differently, so experiment with different quick stress relief techniques to find what works best for you.
Staying grounded. ie keep between +/- 5.
To feel in the present and more grounded, sit on a chair. Feel your feet on the ground and your back against the chair. Notice how your breathing gets deeper and calmer.
Other grounding techniques
• Tap your feet rhythmically 1,2,1,2
• Grab tightly onto your chair as hard as you can.
• Touch various objects around you: a pen, keys, your clothing, or the wall.
• Dig your heels into the floor-literally “grounding” them! Notice the tension centred in your heels as you do this. Remind yourself you are connected to the ground.
• Carry a grounding object in your pocket, which you can touch whenever you feel triggered.
• Notice your body: the weight of your body in the chair; wiggle your toes in your socks; the feel of your chair against your back…
• Stretch. Roll your head around.
• Clench and release your fists.
• Walk slowly; notice each footstep, saying “left or “right”… in detail to yourself.
• Scan the room and notice five things you see in detail.
• Listen for five things that you can hear. The clock ticking, the a/c humming, your own breathing, etc.
• Focus on five things you can feel in contact with your body (ie., your clothes, your back against the chair, your feet on the floor, your hair touching your neck, your watch on your wrist.
• Do the above 3 things simultaneously.
Try This for a week
Tip 4: Don’t isolate
Following a trauma, you may want to withdraw from others, but isolation only makes things worse. Connecting to others face to face will help you heal, so make an effort to maintain your relationships and avoid spending too much time alone.
You don’t have to talk about the trauma. Connecting with others doesn’t have to involve talking about the trauma. In fact, for some people, that can just make things worse. Comfort comes from feeling engaged and accepted by others.
Ask for support. While you don’t have to talk about the trauma itself, it is important that you have someone to share your feelings with face to face, someone who will listen attentively without judging you. Turn to a trusted family member, friend, counsellor, or religious mentor.
Participate in social activities, even if you don’t feel like it. Do “normal” activities with other people, activities that have nothing to do with the traumatic experience.
Reconnect with old friends. If you’ve retreated from relationships that were once important to you, make the effort to reconnect.
Join a support group for trauma survivors. Connecting with others who are facing the same problems can help reduce your sense of isolation, and hearing how others cope can help inspire you in your own recovery.
Volunteer. As well as helping others, volunteering can be a great way to challenge the sense of helplessness that often accompanies trauma. Remind yourself of your strengths and reclaim your sense of power by helping others.
Tip 5: Get moving
Trauma disrupts your body’s natural equilibrium, freezing you in a state of hyperarousal and fear. As well as burning off adrenaline and releasing endorphins, exercise and movement can actually help repair your nervous system.
Move. Go to the loo and breathe, Do the Buddhist walk. Get out of there and calm down.
Exercise that is rhythmic and engages both your arms and legs—such as walking, running, swimming, basketball, or even dancing—works best. Try to exercise for 30 minutes or more on most days. Or if it’s easier, three 10-minute spurts of exercise per day are just as good.
Add a mindfulness element. Instead of focusing on your thoughts or distracting yourself while you exercise, really focus on your body and how it feels as you move. Notice the sensation of your feet hitting the ground, for example, or the rhythm of your breathing, or the feeling of wind on your skin. Rock climbing, boxing, weight training, or martial arts can make this easier—after all, you need to focus on your body movements during these activities in order to avoid injury.
Butterfly Hug Script for Clients
Sit with your back straight. Do abdominal breathing. Imagine you have a little balloon in your stomach that you inflate and deflate, slowly, deeply, smoothly.
Observe what is happening in your mind, emotions and body as you would observe clouds in the sky.
Cross your hands over your chest so that the middle finger of each hand is placed below your collarbone. The rest of your fingers will touch your upper chest. Your hands and fingers are as vertical as possible (pointing more toward your neck than your arms. You can interlock your thumbs.
Alternate the movement of your hands, right, left, simulating the flapping wings of a butterfly.
Continue to breathe slowly and deeply, observing whatever is going through your mind and body (thoughts, images, sounds, odours, emotions and physical sensations) without changing, avoiding or judging anything. Observe it like clouds passing by.
The butterfly is an ancient symbol of transformation. As you use this simple tool, you are facing, rather than avoiding conflict. Whenever you stop avoiding, you raise your level of consciousness (awareness). As you do this, you are strengthening your inner radar detector by becoming more of who you really are, empowering yourself and calming yourself all at the same time.
Treatment for stress
In order to heal from psychological and emotional stress, you may need to resolve the unpleasant feelings and memories you’ve avoided, discharge pent-up “fight-or-flight” energy, learn to regulate strong emotions, and rebuild your ability to trust yourself and other people again.
A variety of different therapy approaches include:
- Talk about your feelings, so you can process them. You need to express how you feel and accept you have the right to feel how you do.
- Somatic experiencing focuses on bodily sensations, rather than thoughts and memories about the traumatic event. By concentrating on what’s happening in your body, you can release pent-up trauma-related energy through shaking, crying, and other forms of physical release.
- Cognitive-behavioural therapy helps you process and evaluate your thoughts and feelings about a trauma.
- EMDR (Eye Movement Desensitization and Reprocessing) incorporates elements of cognitive-behavioural therapy with eye movements or other forms of rhythmic, left-right stimulation that can “unfreeze” stressful and or traumatic memories.
EMDR and the adaptive information processing model .KH 2020
- The theory behind emdr is based on how information is processed in the brain. With happy or everyday events information is processed in an adaptive way
- The brain works like a library. Imagine that an event is like a piece of paper to be filed. It contains details of our thoughts or feelings, the description of the events using all our senses together with our cognitions about the event.
- This is received by the limbic system our emotional brain centre. The limbic system contains the amygdala which is like the smoke detector and detects level of emotional disturbance and the hippocampus which access the librarian. When an event is not too disturbing, the librarian is able to identify relevant hashtags so it can find the relevant brain networks/ files and sub files in the library to the event can not only be filed as a memory but a piece of learning experience. Eg ice cream on a sunny day with mum, #mum, #icecream, #sunshine
- In an everyday event the disturbance isn’t assessed by the amygdala as being too emotional or disturbing so the event is able to be chronologically filed by the as a memory this is how information is processed adaptively.
- However when there is traumatic or distressing event, there is a huge emotional content and so the piece of paper to be filed will be full of fragmented information. There will be huge emotional content and all the senses will be heightened so it cant be written into a coherent storey. This overwhelms the amygdala and so events are not passed as adaptive but maladaptive and therefore not filed.
- Another important factor is the amygdala and hippocampus a timeless, there is no time frame so if information doesn’t get passed to be filed because it’s maladaptive then it will the elements will recur in real time. So you might get flashbacks of the sights or the sounds or triggered by certain elements that have not been filed away.
- So emdr works by kick starting the bilateral ability of the brains natural ability to adaptively process information by taxing the working memory so it no longer can hold emotionally intense data. It enables the original information on your A4 paper to be organised in a way that the brain can process it by working through the fragments and making sense of them, so the client moves from an emotional aroused state to adaptive appropriate emotional grounded state.
What to expect in a session?
Eye Movement Desensitisation and Reprocessing (EMDR) is a treatment whose theoretical base is information processing (i.e. how the brain ‘deals with’ information).
During EMDR the client brings to awareness past and present experiences which are then followed by sets of bilateral stimulation – most usually side-to-side eye movements, but sometimes alternating auditory (sound) tones through a headphone or tactile (touch) sensations through a thumb and finger pad.
Once the eye movements (or alternative) cease, the client is instructed to let material come to awareness without attempting to ‘make anything’ happen. This alternate attention to internal recollections and external stimulus is called ‘dual attention’. This sequence of dual attention and personal association is repeated many times in the session.
What happens in therapy?
The first phase is a history taking session during which the therapist assesses the client’s readiness for EMDR and develops a treatment plan. Client and therapist identify possible targets for EMDR processing. These include recent distressing events, current situations that elicit emotional disturbance, related historical incidents, and the development of specific skills and behaviours that will be needed by the client in future situations.
During the second phase of treatment, the therapist ensures that the client has adequate methods of handling emotional distress and good coping skills, and that the client is in a relatively stable state. If further stabilization is required, or if additional skills are needed, therapy focuses on providing these. The client is then able to use stress reducing techniques whenever necessary, during or between sessions. However, one goal is not to need these techniques once therapy is complete.
Phases three to six involve a target which is identified and processed using EMDR procedures. These involve the client identifying the most vivid visual image related to the memory (if available), a negative belief about self, related emotions and body sensations. The client also identifies a preferred positive belief. The validity of the positive belief is rated, as is the intensity of the negative emotions.
After this, the client is instructed to focus on the image, negative thought, and body sensations whilst simultaneously moving his/her eyes back and forth following the therapist’s fingers (or a mechanical equivalent such as an EyeScan 2000) as they move across his/her field of vision for 20-30 seconds or more, depending upon the need of the client. The kind of dual attention and the length of each set is customized to the need of the client. The client is instructed to just notice whatever happens. After this, the clinician instructs the client to let his/her mind go blank and to notice whatever thought, feeling, image, memory, or sensation comes to mind. Depending upon the client’s report the clinician will facilitate the next focus of attention. In most cases a client-directed association process is encouraged.
This is repeated numerous times throughout the session. If the client becomes distressed or has difficulty with the process, the therapist follows established procedures to help the client resume processing. When the client reports no distress related to the targeted memory, the clinician asks him/her to think of the preferred positive belief that was identified at the beginning of the session, or a better one if it has emerged, and to focus on the incident, while simultaneously engaging in the eye movements. After several sets, clients generally report increased confidence in this positive belief. The therapist checks with the client regarding body sensations. If there are negative sensations, these are processed as above. If there are positive sensations, they are further enhanced.
In phase seven, closure, the therapist asks the client to keep a note during the week to document any related material that may arise and reminds the client of the self-calming activities that were mastered in phase two.
The next session begins with phase eight, re-evaluation of the previous work, and of progress since the previous session. EMDR treatment ensures processing of all related historical events, current incidents that elicit distress, and future scenarios that will require different responses. The overall goal is to produce the most comprehensive and profound treatment effects in the shortest period of time, while simultaneously maintaining a stable client within a balanced system.
After EMDR processing, clients generally report that the emotional distress related to the memory has been eliminated, or greatly decreased, and that they have gained important cognitive insights. Importantly, these emotional and cognitive changes usually result in spontaneous behavioural and personal change, which are further enhanced with standard EMDR procedures.
EMDR: some advice on looking after yourself after the Session
Please note carefully:
The advice below is in addition to advice supplied by your therapist therefore the material below is not intended to be comprehensive or exhaustive. Above all your safety is a key principle. If you have any questions, ask your therapist. You may wish to print this page out as a reminder.
During the EMDR session:
Safety starts in the session itself. Your therapist will help you develop ‘resources’ to promote safety such as resources to help control distressing images, control distressing emotions or promote anything that will help make your journey through EMDR – both in and out of the clinic – as easy and safe as possible.
After an EMDR treatment session:
The effects of EMDR treatment don’t just stop immediately on leaving the clinic! EMDR generates a certain amount of ‘momentum’ to your thinking, emotions, and conscious awareness. You may also experience being slightly light-headed. Rest assured these experiences are quite normal response and fade fairly quickly.
We advise you allow extra time after an EMDR treatment session before returning home or to work.
Try to plan ahead: for instance think how you will return home/to work, are you driving, going by train?
Allow plenty of time, after the treatment session – beware of crossing roads, and concentrate on what is happening ‘now’. Unless your therapist advises differently, approximately half an hour should be sufficient to allow you to concentrate/reference your awareness, back in the present.
It’s strongly advised that you do not drive during this period as you may find your concentration wanders off easily.
On no account put yourself in unnecessary danger. Clients have reported being glad they were more aware than usual when merely crossing the road!
Don’t run to catch a bus or train either. The best way of spending the time is to concentrate on the present – be ‘mindful’ of the present. You could walk around the shops or listen or watch the sights in the city centre, get yourself a tea or coffee, or just sit and relax. York has plenty to be ‘mindful’ of!
Things that may (or may not) happen in the days that follow:
You may just experience a headache after the session. This could be down to not being sufficiently relaxed during the session itself. Remember eyes are moved by muscles and muscles tire easily. Another reason may be that headaches were involved in the target memories you are being treated for.
Make sure you make your therapist aware, extra time can be spent in ‘the closure’ phase to help relax you. Make use of any ‘resources’ developed in treatment and exercises particularly guided visual relaxation. Don’t forget skills you may already have such as yoga, meditation, t’ai chi etc. Actually headaches are not as common as reports of increased dreaming after EMDR. This is nothing to worry about. If you recall your dreams it is likely that they won’t make much sense, with reports frequently saying that dreams “seemed chopped up into pieces”, but there seems little doubt that the frequency of dreaming goes up initially with reports such as “I dreamt from the moment I put my head on the pillow until the next morning”. Other clients report no increased dreaming, indeed sometimes no dreaming at all. Again don’t worry this doesn’t mean the EMDR is not working!
You may become aware of new insights, this is a direct indication that processing is continuing between sessions. Similarly, emotionality can be regarded as important ‘signposts’ for your therapist.
Try to keep a record or log, of these events. Also good advice is to make your partner or significant other aware of any need for support.

 Telephone
Telephone